Varicose Veins: Symptoms, Causes, Diagnosis and Treatment
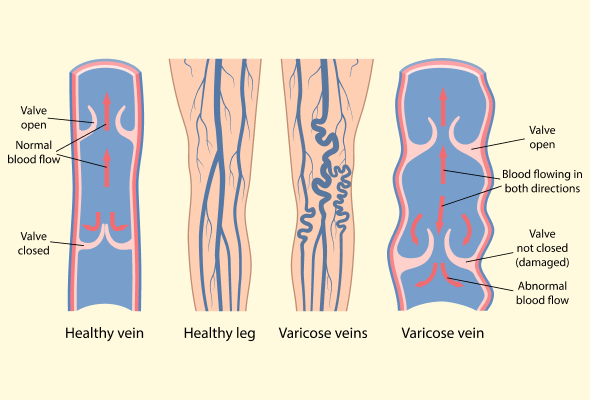
Varicose veins refer to the enlarged, twisted veins that commonly appear on the legs. They look like thick, knotted ropes residing right underneath the skin's surface. When the valves inside the veins stop working properly, blood accumulates inside instead of flowing back to the heart. This causes the veins to swell and take on their characteristic twisted appearance.
Who is likely to get varicose veins?
Several factors contribute to the development of varicose veins, including age, gender (more common in women), family history, prolonged standing or sitting, and obesity.
Symptoms of varicose veins
Some of the common symptoms of varicose veins are:
- Enlarged, purple varicose veins present are the most indicative symptoms. This manifests as twisted, enlarged blue blood vessels clustered beneath lower leg and foot skin, resembling tangled ropes or protruding cords.
- Supplementary spider veins emerge as additional red and blue veins materialising in proximity to varicose sites. These miniature veins populate and spread around adjacent areas surrounding the central enlarged blood vessel.
- A common complaint among sufferers includes heavy, weary, lethargic legs, potentially spanning temporary or chronic durations. Dull aches and more acute soreness specifically concentrated around raised veins may compound heaviness.
- Muscle cramps are a common symptom, and they often get worse at night. Nighttime leg cramps are a common experience for people with varicose veins.
- Varicose veins can cause swelling in the ankles and feet due to fluid buildup in the tissues. If not treated, it can make the swelling worse.
- In extremely untreated cases, the skin may adopt a brownish discolouration or white atrophy. Resultant venous skin ulcers may then open, marking severely damaged surface veins. These additional seldom symptoms require prompt care.
Causes of Varicose Veins
Varicose veins – those swollen, twisted blue lines running down legs – bother almost half of adults at some time. Anyone can develop these unsightly veins, but certain factors increase risks:
- Age:
- As we get older, vein walls progressively lose elasticity while valve flaps inside veins lose their usual tightness.
- This allows blood to leak backwards and pool inside veins, inflaming them.
- By age 50, over half of women and 40-45% of men battle varicose veins.
- Gender:
- Being female comes hand-in-hand with monthly hormone fluctuations and pregnancies, which relax vein walls – both prime triggers for varicose veins.
- This helps explain why women tend to develop varicosities earlier and more commonly than their male counterparts.
- Family Ties:
- If your mom or other close relative has varicose veins, your odds spike too.
- Scientists believe genetics makes vein walls abnormally weak in some families.
- Jobs that Require Standing/Sitting:
- Spending long hours on your feet as a teacher or hairdresser, or sitting for prolonged periods as an office worker can impede proper blood circulation back from the legs affecting the varicose veins along.
The list continues with factors like obesity, bowel issues leading to straining, cysts/tumours blocking good blood flow, tobacco usage, and of course, pregnancy. Understanding common triggers empowers you to minimise risks where possible through lifestyle adjustments.
Diagnosis
To diagnose varicose veins, a doctor examines the legs while the patient is standing to check for swelling. They may inquire about symptoms, such as leg pain and aching. An ultrasound can reveal issues with blood flow and detect blood clots related to damaged leg veins. This non-invasive test uses sound waves to visualise the veins and valves.

How to Treat Varicose Veins
Treating varicose veins may involve self-care, compression stockings, or medical procedures. Outpatient procedures allow most patients to go home the same day. Insurance coverage varies - cosmetic treatment may not qualify.
- Self-Care
- Self-care like exercise, elevating legs, and compression stockings can ease discomfort and progression.
- Walking encourages healthy blood flow.
- Compression Stockings
- Wearing medical compression stockings applies helpful pressure and may prevent worsening.
- Gradient compression stockings are available by prescription if veins cause symptoms.
- Medical Procedures
- If conservative treatment fails, procedures like sclerotherapy, lasers, radiofrequency ablation, vein stripping, or phlebectomy may help.
- All have high success rates for improving appearance and symptoms, but varicose veins can still recur.
How can I prevent Varicose Veins?
Fortunately, adopting some simple healthy habits helps prevent varicose veins:
- Move More
- Exercising energises circulation to efficiently pump blood through veins back to the heart.
- As a bonus, staying active helps in reducing excess weight gain – another varicose vein instigator.
- Aim for at least 30 minutes of daily moderate activity, especially walking.
- Watch Your Weight
- Excess weight pounds veins and forces them to overwork.
- Just a 10-15 pound weight loss eases pressure substantially.
- Focus on fresh, fibre-rich foods served in sensible portions along with regular activity.
- Slimming down not only discourages varicose veins, but boosts energy too.
- Avoid Extended Standing/Sitting
- Prolonged standing or sitting hampers blood circulation back from the legs to the heart.
- Take regular movement breaks to stimulate blood flow and reduce pressure on veins – stand up, march in place, or take a quick walk.
- Change Positions
- Frequently shift positions whether sitting, standing or sleeping to prevent blood pooling in veins.
Conclusion
Varicose veins can cause discomfort, but various treatment options exist, including self-care and medical procedures. Recurrence is possible, especially during pregnancy or due to unhealthy lifestyle choices. However, staying active and maintaining vein health can help prevent onset and reappearance.
For more information visit :- https://www.carehospitals.com/blog-detail/varicose-veins/

Comments
Post a Comment